Since its creation in the federal Income Reduction Act of 2022 (P.L.117-169), Mass Retirees has been closely monitoring the Medicare Drug Price Negotiation Program that the Centers for Medicare & Medicaid Services (CMS) has been administering. In earlier Voice issues, we outlined the process implemented by CMS to negotiate with the manufacturers of ten selected prescription drugs on a maximum fair price (MFP) for each drug.
Most recently in the July Voice, we reported that the negotiations commenced in February and ended this summer( August 1). Then CMS would publish the negotiated MFP for the ten drugs by September 1.
During the six months of negotiations, CMS held three meetings with each participating drug company, attempting to arrive at a mutually acceptable MFP for the selected drug. For five of the drugs, CMS and the drug company reached an agreement on a negotiated MFP for the drug in association. With the remaining five drugs, CMS sent a written final offer to those drug companies, all of whom accepted the final offer. Ed Note: While the Program is ongoing, legal challenges against it continue to be raised by drug manufacturers – without success so far.
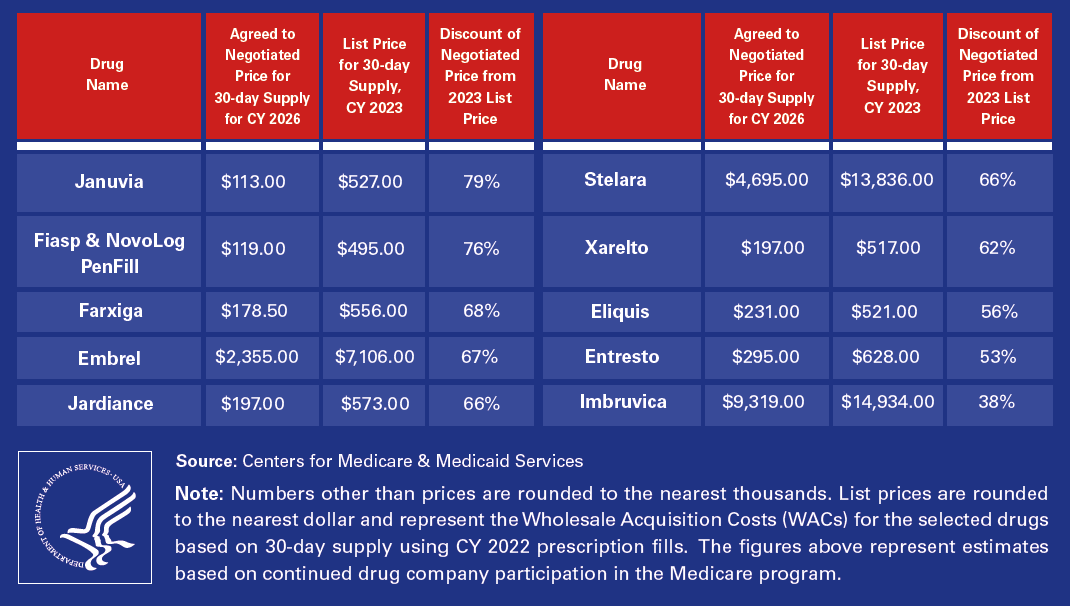
Adhering to its timeline, CMS published the negotiated MFP for the ten selected drugs before the September 1 deadline. (See Table, below.) Beginning now, CMS has six months (until March 1, 2025) to publish its explanation for the MFP of each drug. It must be noted that the drug prices will then become effective on January 1, 2026.
When they do go into effect, it’s estimated that Medicare would save $6 billion in net covered prescription drug costs, which represents a 22% lower net spending in aggregate. Even more important, those enrolled in Medicare prescription drug coverage would save an estimated $1.5 billion.
Remember this represents just the first cycle for the Program with three remaining. An additional 20 Part B or Part D drugs will be selected in years 2027, 2028 and 2029 to take effect in 2029, 2030 and 2031 respectively.