Contains Largely Good News For Retirees
At their May meeting, GIC commissioners focused primarily upon the annual report on out-of-pocket (OOP) costs. After reviewing the highly detailed report, we have determined that it contains largely good news for public retirees and employees insured under the state insurance plan.
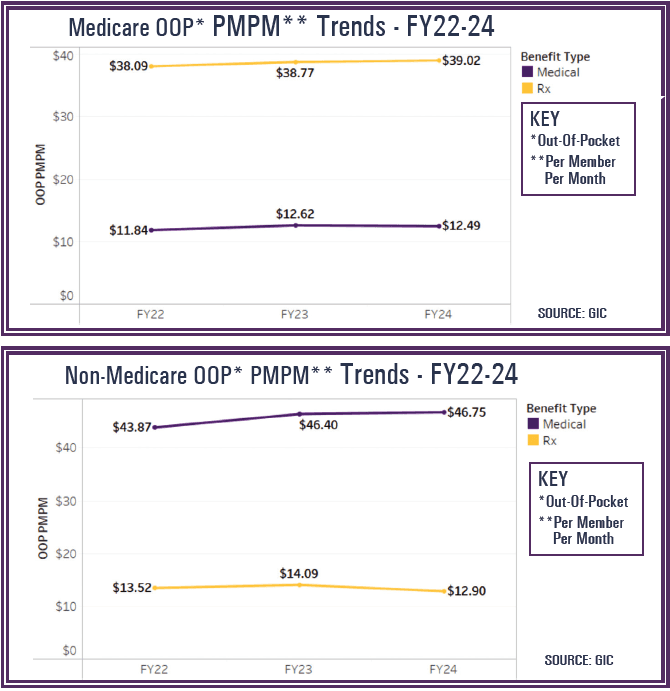
While healthcare costs have continued to rise at an alarming and unsustainable rate, the copayment and deductible burden placed on enrollees by the GIC have not changed in seven years. As the report demonstrates, overall OOP costs per enrolled member remained relatively flat, if not decreased in 2024. See accompanying graphs on Medicare and Non-Medicare OOP (Out-of-Pocket) Trends FY22-FY24.
Despite escalating healthcare costs, the GIC’s commitment to affordability for members continues to deliver results. In FY24, member OOP costs remained stable, even decreased in some areas—while GIC absorbed a significant share of the cost increases driven by medical inflation and rising pharmacy expenses.
Throughout the presentation the staff cautioned that interpretation of FY23-24 trends both on the OOP side and the GIC spend side was complicated by member migration and vendor changes, such as the consolidation of the pharmacy benefit manager, bringing both active and retiree members under the CVS/Caremark/Silverscript umbrella. However, procurement changes did result in some clear examples of savings.
Member OOP Costs: Overall Stability
Some of the report’s key findings on Member OOP costs included the following:
- On the member side regarding OOP costs, there was overall stability with
the Medicare plans, with only minor variations in OOP costs. - For those covered by a non-Medicare plan, there was a slight OOP decrease.
- While there was a nominal increase in medical OOP costs mainly due to
copay alignment and tiering implementation in some plans, despite
higher drug costs overall, OOP dropped by nearly $1.20 Price Per Member
PER Month (PMPM) due to lower generic drug pricing. - CVS/Caremark/Silverscript has a lower allowed amount on maintenance
drugs than Express Scripts had, resulting in a decrease.
Costs Paid by GIC See Moderate Increases
Part of the presentation included a comparison of the costs paid by the GIC alongside the member OOP costs.
The breakdown included data on medical spend and drug spend by the GIC.
In the medical spend category there was a $35.38 PMPM increase from FY23 to FY24. These increases occurred in the broad categories of outpatient and inpatient surgical, inpatient medical, outpatient psychiatric and pharmacy.
The report yields some interesting data in the prescription drug spend category. Brand drugs were up approximately $15.00, led by GLP-1 utilization for diabetes and weight loss. It was noted that there are 11K utilizers on non-Medicare plans accounting for a drug spend of $15M monthly GIC cost. The OOP member cost is $30 (30-day), $75 (90-day). The increase in the brand drugs was offset by $1.43 decrease in specialty drugs due to biosimilars for Humira and CVS Caremark made changes to the formulary in April 2024.
Spending Compared to Other Plans
Another valuable aspect of the report is the comparison to other plans in the Massachusetts marketplace. Utilizing data from the Center for Health Information and Analysis (CHIA) the staff compared the GIC spend to those plans in the Jumbo Group, defined as 500+ employees.
Two interesting data points were highlighted.
- The GIC percentage of medical cost share is calculated at 91.6%. This has
remained stable over the last three fiscal years. However, it was noted that
the jumbo group runs around 89%, slightly lower than the GIC. - The data also indicated that 31% of large employers increased cost sharing
in 2024 as a mechanism to address cost, GIC and most municipal plans did not.
“As we see it, the GIC OOP report continues to provide very important data,” comments Association’s Nancy McGovern. “It will be a valuable resource as we continue to examine solutions to rising healthcare costs.”



